Restless Leg Syndrome Treatment
Symptoms of Restless Leg Syndrome

Patients with Restless Leg Syndrome (RLS) experience uncomfortable sensations in their legs, especially at night. Patient reports vary, and can include “itchy,” “creepy-crawly,” or “pins and needles” feelings. These symptoms are accompanied by a strong, nearly irresistible urge to move the legs. This understandably makes it difficult to fall asleep and stay asleep, making disrupted sleep the hallmark symptom of RLS.
Symptoms vary between patients, ranging from barely noticeable to debilitating. While not harmful in its own right, Restless Leg Syndrome has great potential to lower a patient’s overall quality of life. For many sufferers, severe sleep disruption causes chronic exhaustion which affects many aspects of their physical and mental health.
What does a typical Restless Legs Syndrome (RLS) patient look like?
Restless Leg Syndrome is observed in about 10% of American adults. Anyone may have RLS, even small children. However, the most severe cases tend to occur in females over the age of 30.
This condition is often misdiagnosed, especially in younger children and those with mild symptoms. Only when RLS is diagnosed correctly can successful treatment begin.
Causes of Restless Leg Syndrome
To date, no single cause of RLS has been identified, yet there appears to be a genetic component. About 50% of RLS patients have a relative who is also affected.
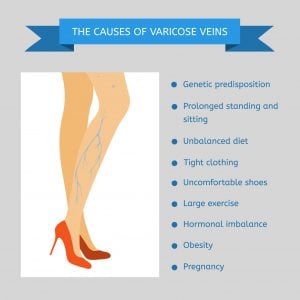
Other suspected causes, as well as factors which may aggravate the condition, include:
- Certain chronic diseases and dietary deficiencies. Although we don’t know why, RLS is found at much higher rates in those with Parkinson’s disease. Diabetics, especially those with peripheral neuropathy, also have elevated rates of RLS, as do patients with kidney failure. Research has also demonstrated that chronic iron deficiency can increase RLS symptoms. Symptoms often abate when the underlying condition is treated or well-managed.
- Some types of medication. Allergy medications in the antihistamine class such as Benadryl (diphenhydramine) may make RLS symptoms worse. Antidepressants such as Effexor (bupropion) and antipsychotics such as Haldol (haloperidol) may also aggravate RLS symptoms.
- Pregnancy. It’s unknown why, but pregnant women experience RLS much more often than the general population. This is especially true during the 3rd trimester. Symptoms generally improve after delivery.
- Excessive alcohol consumption. Drinking too much, especially before bed, can make RLS symptoms worse in some patients.
- Sleep deprivation. This is another factor known to aggravate RLS. This can become a self-perpetuating cycle, with RLS symptoms causing sleep deprivation which in turn contributes to RLS.
Diagnosing Restless Leg Syndrome (RLS)
Often, patients come to their doctors complaining of excessive daytime sleepiness, and may themselves suspect RLS. While medical tests might be done to rule out other conditions, no medical tests or bloodwork can diagnose RLS. Instead, the diagnosis is made clinically, based on symptoms and a patient’s medical and family history. A thorough review of a patient’s medications is taken into account as well. The overall health and lifestyle of each patient must be considered before a final diagnosis is reached.
Restless Leg Syndrome Treatment
Just as there isn’t one single cause of RLS, no one treatment is able to “cure” it. As such, most treatment protocols are aimed at easing symptoms. Often, this involves simple lifestyle changes as opposed to medications.
This is especially true for mild-moderate symptoms. Often all that’s required to reduce or even eliminate symptoms is limiting caffeine intake and establishing a regular sleep schedule. Other lifestyle modifications used to successfully treat RLS include limiting alcohol intake, stopping tobacco use, and engaging in regular exercise. Treatment of other sleep-disrupting conditions such as sleep apnea (snoring) can also help.
The following are other drug-free methods which provide some patients relief:
- Deep tissue leg massage
- Applying hot packs to the legs
- Soaking in a hot tub or taking warm baths.
- Applying ice packs to the legs or soaking the them in cold water
- Avoiding daytime naps in order to establish a better sleeping schedule
- Specialty vibration pads such as the Relaxis device.
Drug therapy can be helpful if these conservative methods fail. No single medication has been found which helps all RLS sufferers, however. In fact, a drug which provides relief in one patient may exacerbate symptoms in another. Tolerance is also a concern. Even if a medication works, it’s possible for it to lose its effectiveness if used for long periods.
Common medications prescribed for RLS include:

- Dopaminergic drugs: these medications act on the neurotransmitter dopamine. Currently, the drugs Requip, Mirapex, and Neupro are approved for treating mild-moderate RLS. Again, note that these drugs are not effective in all patients. Levodopa isn’t FDA approved for RLS, but is sometimes used off-label.
- Benzodiazepine sedatives: these are a group of anti-anxiety drugs which includes Xanax, Ativan, and Valium. These may cause excessive daytime sleepiness. A high potential for abuse and addiction is also a concern with these drugs.
- Narcotic pain medication: usually used only for moderate-severe pain, drugs such as Vicodin and Oxycodone have shown some effectiveness in treating RLS. Much as with benzodiazepines, the potential for abuse limits their usefulness.
- Antiepileptic drugs: drugs such as Horizant, Neurontin, Lamictil, and Tegretol are usually used to treat seizure disorders. They’ve also shown to be helpful in some patients with RLS.
Choosing a medication to treat RLS is often done by a process of trial and error. It’s a matter of finding the drug which best manages symptoms and improves sleep quality while having the fewest adverse effects.
Lifestyle modifications and DIY remedies
If your RLS is minor, changing your way of living can be your only treatment.
RLS symptoms could potentially be avoided by:
- decreasing your consumption of nicotine, caffeine, and cigarettes, which are frequently used as RLS symptom triggers.
- ensuring that your diet has enough iron or taking supplements (some studies have linked iron deficiency to RLS)
- reviewing your prescriptions with your physician and maybe switching any that might be causing RLS
- doing regular exercise
- Distracting yourself when you have to sit still by doing things like talking to people, needlework, or playing video games
The International Restless Leg Syndrome Study Group:
As per the above academic research group, the “classic” symptoms of RLS include:
- A “crawling” or “creepy-crawly” feeling deep within the legs. This may occur in the arms as well, but this is much rarer.
- Itchy, tingling, or “pins and needles” sensations in the legs.
- An irresistible urge to rapidly move the affected limbs.
- Generalized restlessness in the absence of symptoms. This can include tossing and turning, floor pacing, and sleeplessness.
These symptoms may occur during the day but are typically at their worst at night when lying down. They are usually relieved by activity, such as getting up and walking around. This is why floor pacing is common among RLS patients. In extremely severe cases, symptoms may be constant, and are not relieved by lifestyle changes, activity, or medication.
Does RLS lead to Other Sleep Disorders Like Insomnia Or Sleep Apnea?
Yes, unfortunately having restless leg syndrome increases your chances of developing some other sleep related disorders such as sleep apnea and insomnia. The continuous urge and discomfort to move legs can lead to sleep deprivation, which leads to insomnia.
Fortunately, RLS directly can’t cause sleep apnea, but it can contribute in the development of sleep apnea. Since both conditions are known to disturb sleep cycles, which leads to poor quality of sleep and even daytime fatigue. That’s why it’s important to get the right treatment before RLS gets worse and cause you even more sleep related problems.
Is RLS More Common in Women Compared To Man?
Unfortunately yes, women are more likely at a risk of restless leg syndrome than men. Sadly, the reason behind this isn’t fully understood but it could be because of hormonal changes, especially during the pregnancy since many women experience restless leg syndrome during pregnancy and menopause could also play a role in this condition. However, always remember restless leg syndrome can happen to. Anyone, whether men or women and it gets worse with age.
Can Restlessness Leg Syndrome Affect Any Other Body Part Other Than Legs?
Yes, while it’s true restless leg syndrome affects mainly legs, it might spread or develop in other body parts too, some of these parts can include:
- Arms: The same discomforting and uncomfortable sensations and urge can appear in hands, but it’s more manageable than legs.
- Torso: In rare cases, RLS sensations may extend to the torso and can lead to discomfort in the chest and abdomen.
- Face: Although extremely uncommon, in some cases tingling in face has been reported.
- Feet: Feet are the closest thing to legs, so it’s really obvious for it to spread there and cause disturbance.
“Non-classic” RLS symptoms can include:
- Excessive daytime drowsiness
- Chronic fatigue
- Involuntary jerking leg movements which occur when a patient is awake. These are known as Periodic Limb Movements (PLMs), and are observed in about 90% of patients with RLS.
Not everyone with RLS experiences symptoms every night. Some individuals have only one or two episodes a month, and others may go for months with no symptoms. It is unknown at this time why such remissions occur, or what triggers the disorder again.
It was previously thought that RLS was caused by vascular disease or nerve damage in the legs. While vein disease (venous reflux) is known to contribute to RLS, research has yet to conclusively link nerve damage to RLS.
Patients with diabetic neuropathy do experience RLS symptoms with greater frequency than the healthy population. However, no connection between the sensory nerve damage found in diabetic neuropathy has been established. Instead, these elevated rates appear to be due to other factors common to diabetic patients, especially vein disease.
Imbalances in certain chemical messengers in the brain known as neurotransmitters may be involved in RLS. These help regulate movement, and could potentially lead to involuntary movements such as those found in RLS. Current research is being done to investigate this connection.