Tendonitis foot treatment

Tendonitis Foot Basic Information:
Tendonitis foot treatment 
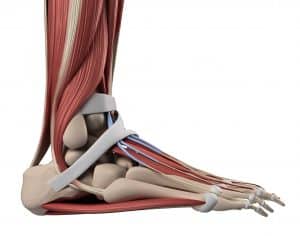
The large tendon which connects your heel to your calf muscles, the Achilles tendon, is a common site of injury. Tendon injury also occurs relatively frequently to the medial (inside) and lateral (outside) tendons of the ankle. For detailed descriptions of these injuries, search the terms Achilles Tendonitis, ankle sprain and sports injuries.
This overview deals with less severe injuries, not full tears or ruptures. This type of injury is by far the most common type of tendon injury, affecting millions of people each year in America and around the world. These are extremely common sports injuries, yet can happen to anyone.
Tendonitis, tendinosis, and tendinopathy:
A tendon injury is possible anywhere a muscle inserts into a bone, and commonly occur near a joint. The shoulders, knees, elbows, and ankles are especially vulnerable, and the bulk of tendon injuries occur in these areas. This type of non-tear injury doesn’t happen suddenly, and is instead usually the result of chronic micro-trauma, also known as “wear and tear.” By and large, these are overuse injuries.
Here are the basic technical terms for this type of injury:
- Tendinitis: this term is used to describe chronic inflammation of a tendon.
- Tendinosis: This term describes micro-trauma in the form of many tiny tears throughout the length of the tendon.
- Tendinopathy: A general term which simply means a medical condition affecting a tendon.
In a clinical setting, doctors tend to use the term “tendonitis” to describe many types of tendon injuries. Today, the terms “tendinosis” and the more general “tendinopathy” are rarely used by non-specialist physicians.
How are tendons injured?
As mentioned, these injuries are most often due to chronic overuse, and are more common in older and very active individuals. They also frequently occur in sports and professions where the same motions are made regularly for weeks, months, and years. T
In cases of sudden tendon injury, it is highly likely that the injured tendon was being gradually weakened over time. In this vulnerable state, a major tendon injury can occur much more easily.
Symptoms of a tendon injury:
- Pain tends to worsen with active movement (muscle contraction moving a joint). There is less pain when the joint is being moved by someone else, for example a doctor examining the injured joint.
- Pain and stiffness is usually worse in the morning until the patient “warms up.” Symptoms also tend to worsen at night, after the patient has been using the joint throughout the day.
- There is usually visible swelling and inflammation. The area may be tender and warm to the touch.
- A crunchy sound and a grinding feeling is common when using the joint which the tendon crosses.
- In many ways, the symptoms of a tendon injury are similar to those of bursitis. A physical examination by a trained healthcare professional is usually needed to tell them apart. Imaging tests such as CT scans and MRIs are also useful.
Diagnosing a tendon injury:
Your doctor will start by taking a medical history, followed by questions about how the injury occurred and what symptoms you’re experiencing. This will be followed by a physical exam including orthopedic tests. Your doctor will bend the joint in different directions to determine what structures have been damaged. While these tests are low tech, they are quite useful and often
provide the information needed for a diagnosis.
If there’s any doubt, or if your symptoms don’t improve with time and conservative treatment, further exams are needed. This usually includes some type of imaging, whether it be an X-Ray exam, CT scan, or MRI.
Diagnostic tests and exams for diagnosing tendon injury:
In most cases, imaging exams aren’t necessary to diagnose a tendon injury. Instead, the diagnosis is made based on the patient’s history and physical exam. Orthopedic tests, in which the doctor stresses the suspected tendon, can be very useful (and are often more accurate than imaging studies). While things like observing range of motion and testing muscle strength aren’t technically orthopedic tests, they’re very useful nonetheless.
Further testing is needed if there’s any doubt about the diagnosis or if symptoms fail to improve with time and treatment. This is where imaging tests come into play, including:
- X-ray studies. These can’t visualize tendons and other soft tissue structures well, but are very good at identifying calcium deposits. This is often enough to reach a diagnosis. They’re also inexpensive, which makes them a good place to start when diagnosing musculoskeletal injuries.
- Ultrasound exams. While ultrasound can’t penetrate bones, it’s capable of showing small tears within ligaments and tendons. Unlike X-ray exams, ultrasound is completely safe since it doesn’t involve radiation. It’s also a very cost effective option.
- MRI (magnetic resonance imaging) exams. MRI is the standard by which all other imaging exams are judged. They can visualize all types of tissues, including tendons, ligaments, muscles, bones, and organs. The level of detail achievable with MRI is unmatched. At this time, MRI studies are very expensive.
What is the role of ice and heat therapy in the management of tendonitis?
Ice and heat therapy can play different roles in the management of tendonitis. Here’s a breakdown of their roles:
- Ice Therapy (Cold Therapy):
Ice therapy is commonly used during the acute phase of tendonitis, especially when there is inflammation and swelling. The application of ice helps reduce blood flow to the affected area, numbs the area, and decreases tissue metabolism, thereby reducing pain, inflammation, and swelling. Ice packs or cold compresses are typically applied for about 15-20 minutes at a time, several times a day. It’s important to use a barrier, such as a cloth or towel, between the ice pack and the skin to prevent ice burns.
- Heat Therapy:
Heat therapy is generally applied during the subacute or chronic phase of tendonitis when inflammation and swelling have subsided. Heat helps improve blood circulation, relaxes muscles, and promotes healing. The increased blood flow can deliver essential nutrients and oxygen to the affected area, aiding in tissue repair. Heat can be applied through warm compresses, hot water bottles, heating pads, or warm baths. It is usually recommended to use heat for around 15-20 minutes at a time, a few times per day.
It’s Important to note that the choice between ice and heat therapy depends on the stage of tendonitis and the individual’s response. Some people find more relief with ice, while others prefer heat. It can be helpful to experiment with both and determine which therapy provides the most effective pain relief and comfort for an individual’s specific case of tendonitis.
How long does it typically take for tendonitis to heal with proper treatment?
The healing time for tendonitis can vary depending on various factors such as the severity of the injury, the affected tendon, and individual healing abilities. With proper treatment, it may take several weeks to a few months for tendonitis to heal completely.
Treating a tendon injury:
In less severe cases, your injury may be treatable at home under your doctor’s general guidance. Start the following as soon as possible after you begin experiencing symp
Overview of treatment for tendon injuries:
Initial treatment for tendinopathy, the catchall term for tendon injuries, is fairly straightforward. This typically involves relative rest, e.g. “taking it easy,” and over the counter pain medications. NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) such as Motrin and Aleve are recommended to reduce swelling. Gentle, non-weight bearing range of motion exercises are also a good idea.
The goals of this initial treatment period are simple:
- Limit excessive inflammation and swelling
- Manage pain
- Rest to allow healing to begin
If your injury doesn’t respond to this conservative treatment, you’ll probably be sent to physical therapy. This can be highly effective, and some doctors prescribe PT as a matter of course for all tendon injuries. If your tendon injury is due to repetitive motion (which most are), your physical therapist can help you find more biomechanically correct ways to perform this motion. The basic goals of physical therapy are:
- Reducing pain
- Restoring full range of motion, if needed
- Restoring joint stability, if needed
- Developing strength and coordination of the muscles surrounding the injured tendon. This is one of the best ways to prevent re-injury in most musculoskeletal injuries
- Encourage complete healing of the tendon
How does tendonitis in the foot affect overall mobility and daily activities?
There are variety of ways in which tendonitis in foot can affect your overall mobility and daily activities, because after all it’s a foot problem which should be obvious since feet are one of the most important parts of body, so let’s see how it will affect you:
1. Pain and Discomfort
Tendonitis causes pain in the affected tendon which can make many foot related activities painful, whether it’s walking, standing, exercises or other weight bearing activities, as long as there’s pressure on the tendon you will experience pain. The discomfort can vary from mild to severe which can affect your daily tasks.
2. Limited Movement
Just like many injuries, Tendonitis pain can limit your fool’s movement as it might cause more inflammation when moved in a certain direction, which restricts movement, making many activities difficult.
3. Change In Gait
Many people change the way they walk whenever they have foot injury, it can happen unconsciously to avoid pain, leading to an altered gait. Which isn’t a really great idea, since doing so can put strain on other body parts like knees and back, leading to discomfort in those areas as well.
4. Mental Impact:
Continuous pain, not being able to move freely, and change in gait can easily lead to stress and frustration, especially if your works requires moving a lot. Which in result might even lead to depression and anger.
When should you see a doctor for tendonitis in the foot?
There are several signs that can help you identify it’s the best time to visit a doctor, here are some of them:
1. Severe symptoms: If you experience serious symptoms like extremely pain, swelling, and redness.
2. No improvement: If you see no improvement in pain, healing and swelling after self care.
3. Difficulty in walking: If your work requires a lot of moving, you shouldn’t even wait, as walking can be painful.
Tendinitis, Tendinosis, and Tendinopathy.
The Terminology of Tendon Injury
Doctors, nurses, and other healthcare professionals speak a different language from the rest of us. While it can certainly be confusing for the uninitiated, this complexity makes sense when considering its purpose.
Medical terminology is primarily used by doctors and allied health professionals to talk to one another. It’s also the language of medical research. It’s designed to allow clinicians to describe highly detailed concepts and information in an efficient, precise, and unambiguous manner.
So with this in mind, let’s look at the surprisingly imprecise medical terminology surrounding tendon injuries. It’s a not entirely rare and very teachable case of technical medical terminology used in a technically incorrect manner. Concerning tendon injury, there’s a big difference between what’s in the textbook versus what practitioners actually say in clinical practice.
Tendinitis
—note that “itis” is the medical suffix meaning “inflammation.” You’ve almost certainly heard this root before. For example, appendicitis is the inflammation of the appendix, while tonsillitis is the inflammation of the tonsils. Thus, Achilles tendinitis is chronic inflammation of this tendon that’s severe enough to cause physical symptoms such as pain.
Also note that, while specific to inflammation-driven tendon conditions, most specialists use the term “tendinitis” very loosely. It’s become more of a general term which refers to a wide variety of tendon injuries, regardless of what causes them. For many professionals it’s become a shorthand for tendon problems in general (see “tendinopathy”).
Tendinosis
—note that “osis” is the medical suffix referring to a “process” or “state,” usually diseased. It’s not meant to be an overly specific term. Yet medical researchers have nevertheless used it to describe the structural breakdown of tendon tissue in overuse injuries.
Doctors, nurses, and other healthcare professionals speak a different language from the rest of us. While it can certainly be confusing for the uninitiated, this complexity makes sense when considering its purpose.
Medical terminology is primarily used by doctors and allied health professionals to talk to one another. It’s also the language of medical research. It’s designed to allow clinicians to describe highly detailed concepts and information in an efficient, precise, and unambiguous manner.
So with this in mind, let’s look at the surprisingly imprecise medical terminology surrounding tendon injuries. It’s a not entirely rare and very teachable case of technical medical terminology used in a technically incorrect manner. Concerning tendon injury, there’s a big difference between what’s in the textbook versus what practitioners actually say in clinical practice.