Rheumatoid Arthritis

Rheumatoid Arthritis
Other names: Inflammatory Joint Disease, Arthritis
What is rheumatoid arthritis?
Rheumatoid arthritis (RA) only affects about 1% of adults living in the U.S., which is about 2.1 million people. While RA mostly presents in patients over the age of 40, it may present at any point in a person’s life. Rheumatoid arthritis is an inflammatory disease, known for causing pain, stiffness, swelling, and loss of function in the afflicted joints. Typically, rheumatoid arthritis will affect both sides of the body symmetrically, so if you are experiencing symptoms, you should expect to experience them in the other ligament. Additionally, RA will tend to feel worse in the mornings. Finally, rheumatoid arthritis can affect not only joints, but also the organs.
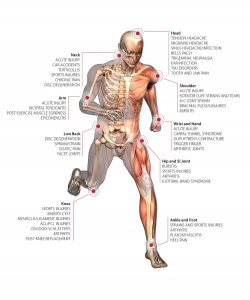
What are the symptoms of rheumatoid arthritis?
 Red, hot, tender joints
Red, hot, tender joints- Stiffness, even if the joint isn’t being used
- Nodules around the elbows
- Deformities in the joints
- Swelling in the joints
- Bunions, foot pain, and hammer toes (in later stages)
- Fever and lack of appetite and energy
What causes rheumatoid arthritis?
Rheumatoid arthritis is an autoimmune disease (the body attacking itself). So far, scientists still do not know exactly what causes the immune system to react this way with this particular condition, but recent research points to the following causes:
Rheumatoid arthritis is an autoimmune disease, which means that it is a disease where the body begins to attack itself. Research has yet to provide any information as to why the body’s immune system begins to attack itself, but so far signs tend to point to the following causes:
- Genetic or inherited factors.
- Select environmental factors; viruses or bacteria could be the cause, but these are not the ones typically associated with common communicable diseases such as the flu or the common cold.
- Hormones may play a factor, as certain situations where hormones are adversely affected, such as pregnancy, can lessen the effects, whereas women who are breastfeeding can experience painful flare-ups of rheumatoid arthritis.
How does my doctor tell if I have rheumatoid arthritis?
Unfortunately there are no single tests to take in order to determine whether or not you have RA, and attempts to diagnose the disease in the early stages can prove to be futile, as the symptoms differ greatly from person to person in these stages. Additionally, the signs can look similar to other types of arthritis. When trying to determine your situation, your physician may use the following steps to see if you have rheumatoid arthritis:
- The first thing they will likely do is take a medical history, in which they will ask about the progression of the symptoms, as well as all oddities that have plagued the patient within a reasonable passage of time.
- Second, they will perform a physical examination, looking for abnormalities in the tendons that present on the surface, as well as testing the functionality of the patient’s motor skills.
- If deemed necessary, they may order tests for rheumatoid factor, an antibody commonly found in patients suffering with rheumatoid arthritis. Other tests may also be ordered.
- Once it is determined that the disease is present, X-rays will be ordered to see the extent of joint damage.
How is rheumatoid arthritis treated?
In order to effectively treat RA, your physician will help tailor an effective treatment program that suits your lifestyle and effectively addresses your needs.
Rheumatoid arthritis generally tries to accomplish four goals:
- Alleviate pain
- Reduce inflammation
- Halt or slow down joint damage
- Restore sense of autonomy in the patient, and help them feel in control of their life again
Non-surgical treatments
Exercise
 Exercise: One of the best treatment possibilities for patients to pursue is an increase in exercise. Working out can help in a multitude of ways, including providing an improvement of mood, a decrease in pain, strengthening of the heart, and improving general physical fitness. Another perk is that it is relatively inexpensive and, with proper guidance, will have very few negative results. When planning your exercise regime, your physician will aim to utilize problem areas in safe and productive ways.
Exercise: One of the best treatment possibilities for patients to pursue is an increase in exercise. Working out can help in a multitude of ways, including providing an improvement of mood, a decrease in pain, strengthening of the heart, and improving general physical fitness. Another perk is that it is relatively inexpensive and, with proper guidance, will have very few negative results. When planning your exercise regime, your physician will aim to utilize problem areas in safe and productive ways.
Rest
Rest and joint care: Resting is vitally important in the healing process, and when you aren’t actively exercising the affected areas the extended breaks can work wonders for the body as a whole. When recovering, patients should learn the tell-tale signs of their bodies that let them know it is time to take a break and relax. Resting can be as simple as staying off your feet, but could also be the use of canes, braces or splints to support the body and minimize the strain on the body. Your doctor should be the one to recommend resting options based on your needs, however it is important that you voice concerns and talk it out with them to ensure proper healing.
pain relief
Non-drug pain relief: It is possible to find relief without the use of medication; warm towels, heat packs, and or a warm shower/bath will often be used to alleviate pain and stiffness. Conversely, cold treatments can also relieve pain or numbness, but it is up to your physician to determine which treatment is best for you. Therapy pool sessions can also be beneficial, as the water helps reduce the effect of gravity on your body, in addition to warming and treating the affected areas. For rheumatoid arthritis affecting in the knee, patients can wear insoles that redistribute weight, reducing joint stress.
Weight Control
Weight Control: Weight can play a factor in the severity of the disease, and shedding a few pounds can lessen the stress on the weight-bearing joints. Ask your physician what kinds of dieting plans and exercise regimens could help benefit you the most.
Stress reduction
Climate and stress reduction: While sudden changes in the weather can have adverse effects on patients suffering with rheumatoid arthritis, research seems to suggest that a move to an area with controlled climates does not improve the condition. Stress from work or family is however a concern that can be alleviated with some lifestyle changes. Having a healthy discussion with family about the limitations that the patient may experience can help build a strong foundation of support, while also cementing aspects of their life where they expect independence.
Medicines
 Medicines: Physicians can prescribe medical treatments to reduce inflammation and/or pain. When selecting the right kind of treatment, physicians will often consider a few variables in the progression of the disease, such as the level of pain and potential for side effects of medicating. When medicating, patients should always consult with their physicians about any medications they are already taking, and report any changes to their body.
Medicines: Physicians can prescribe medical treatments to reduce inflammation and/or pain. When selecting the right kind of treatment, physicians will often consider a few variables in the progression of the disease, such as the level of pain and potential for side effects of medicating. When medicating, patients should always consult with their physicians about any medications they are already taking, and report any changes to their body.
Rheumatoid arthritis can be treated with a variety of medications, but it is important to consult a physician about which drugs can be most beneficial. Some of the following medications may be offered to help treat the symptoms of the disease.
Medicines
- Disease-modifying antirheumatic drugs (DMARDs) are painkillers specifically targeted to help swollen joints and halt joint damage. While their effects may not be noticable for a time up to a few months, or as short as a few weeks, patients can experience drastic improvements in their affected areas.
- Aspirin is a common remedy that lowers swelling and inflammation, while also reducing pain. It allows patients more freedom of movement and can help make day-to-day activities more bearable. Aspirin use is generally part of early treatment.
- Acetaminophen, the active ingredient in many common pain relievers such as Tylenol™ can be used to help deal with some of the symptoms. While it does not reduce inflammation, it doesn’t carry some of the severe side-effects, and is easier on the stomach.
- NSAIDs (nonsteroidal anti inflammatory drugs) are over-the-counter drugs such as aspirin, Advi™l, Motrin IB™, ketoprofen, Aleve™, as well as a few prescription medications can help with symptoms. COX-2 inhibitors, and newer NSAIDs such as Celecoxi™ and Celebrex™ can reduce inflammation.
- Biologic response modifiers selectively block parts of the immune system called cytokines. Cytokines play a role in inflammation. Long-term efficacy and safety are uncertain.
- Biologic response modifiers can selectively block cytokines, a part of the immune system that plays a role in inflammation. This is still a relatively new treatment and its long-term results are uncertain.
- Oral corticosteroids should not be used to treat RA.
Brand names
*Brand names that were included in this section are for user friendliness and understandability. Beaver Valley Foot Clinic does not endorse nor suggest that its readers use any of these products without consulting with a physician first. If a product is not listed here that does not imply that they are ineffective at treating rheumatoid arthritis.*
Most RA medications come with potential side effects, and it is important that patients learn what side effects they should look out for from the treatments they are prescribed. Nonperscription medications can also yield side effects, so it is important to research them as well. NSAIDs can have a higher risk of side effects in certain individuals, such as those with a history of peptic ulcers or digestive tract bleeding, those taking oral anticoagulants or corticosteroids, smokers and those who regularly consume alcohol. These side effects can be mitigated by reducing gastric irritants such as alcohol, tobacco, and caffeine, while also taking their medications with food. There are medications that can help coat the stomach lining to mitigate the effects of the RA medications, however these methods are not always completely effective.
Surgical treatments
There are surgical options to help with severe joint damage, however, the cost/benefits surgery must be weighed beforehand. Several surgeries include:
 Hammertoe Surgery: hammertoes can be fixed with a simple, minimally invasive, 15-minute office procedure. The toe’s contracted tendons are reduced, the toe is straightened.
Hammertoe Surgery: hammertoes can be fixed with a simple, minimally invasive, 15-minute office procedure. The toe’s contracted tendons are reduced, the toe is straightened.
Joint replacement: Joint replacement surgery is the most frequently performed surgery to treat RA. It can help relieve pain and improve or restore joint function, however, the surgery will often have to be repeated, as the artificial joints are not always permanent.
Tendon reconstruction: If the damage to the tendons is severe enough, surgery can be done to reconstruct the tendons by attaching an another tendon to it. This is mostly done in the hands, and can often restore significant function to the hand.
Synovectomy: This type of surgery is seldom suggested, as it is not able to fully remove the inflamed synovial tissues that are causing issues.
Nontraditional approaches
We highly suggest talking with your physician before starting any kind of alternative forms of therapy, such as acupuncture, herbal supplements, and/or special diets.
What are the risk factors for developing RA?
The exact cause of Rheumatoid Arthritis (RA) is unknown, but several factors can increase the risk of developing the condition. Common risk factors for RA include:
- Genetics: A family history of RA or other autoimmune diseases increases the risk.
- Gender: Women are more likely to develop RA than men.
- Age: Although RA can begin at any age, it often starts between the ages of 30 and 60.
- Smoking: Smoking tobacco increases the risk, especially in people with a genetic predisposition.
- Environmental Exposures: Prolonged exposure to certain environmental factors, such as asbestos or silica, can increase the risk.
- Obesity: Being overweight or obese can increase the risk and severity of RA.
- Hormonal Factors: Hormonal changes, such as those occurring during pregnancy, might affect the immune system and contribute to RA development.
Can children develop Rheumatoid Arthritis?
Yes, children can develop a form of arthritis known as Juvenile Idiopathic Arthritis (JIA), which is the most common type of arthritis in children. JIA is an umbrella term that includes several subtypes of arthritis, one of which is similar to adult Rheumatoid Arthritis (RA) and is referred to as Juvenile Rheumatoid Arthritis (JRA) or Juvenile Idiopathic Arthritis associated with Rheumatoid Factor (RF-positive JIA).
JRA shares some similarities with adult RA, such as joint pain, swelling, and stiffness. However, it affects children under the age of 16 and often presents differently than RA in adults.
What complications can arise from uncontrolled RA?
Uncontrolled Rheumatoid Arthritis (RA) can lead to several complications, including:
- Joint Damage: RA can cause severe joint damage and deformities, leading to loss of mobility and function.
- Chronic Pain: Persistent pain and discomfort can significantly affect the quality of life.
- Disability: Severe RA can result in disability, making it challenging to perform everyday tasks.

 Red, hot, tender joints
Red, hot, tender joints