Gout Treatment & Symptoms

Do Podiatrists Treat Gout? – Yes, Podiatrists best Doctor for Gout in Big Toe !

What is Gout?
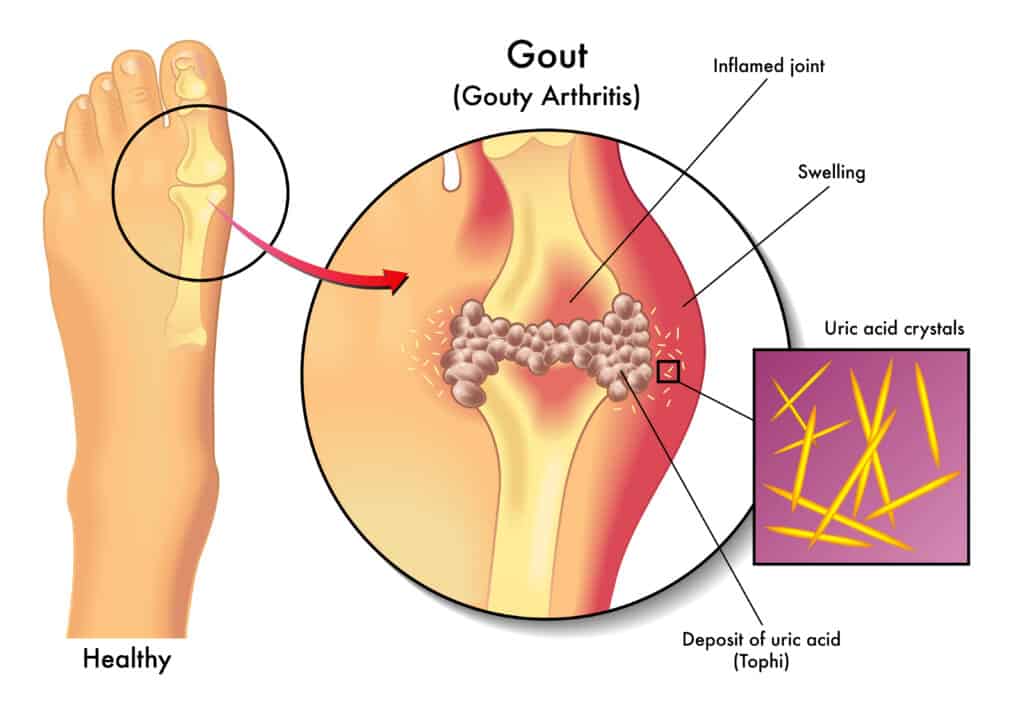
Gout is when an overabundance of uric acid is present in the body. Gout treatment is vital, as multiple organs can be damaged. This high level of uric acid results from either producing too much or excreting too little. Gout is the term to describe this condition whether it is acutely or chronically present.
Individuals with gout typically experience symptoms affecting the feet such as swelling, pain, redness, particularly in the joint of the big toe. Acute gout is accompanied by sporadic attacks that affect most major extremity joints, with small joints of the hands and feet most affected.
Chronic gout caused hard swellings known as tophi that form on the joints. They are made of uric acid and have the possibility to grow very large and even to the point of breaking through skin. One or more of the following treatments may be used by individuals who suffer from gout.
Gout Treatment
Step by step, Podiatrists are the best doctors to treat gout.
- First talk to a podiatrist who specializes in the treatment of gout in the foot. Since 90% of gout happens in the foot, Podiatrists are some of the most well versed physicians when it comes to gout treatment in the big toe joint, the foot and ankle.
- Prescription Colchicine helps reduce the Uric Acid load through the kidneys.
Podiatrists are able to prescribe all available immediate pain relief medications such as anti-inflammatories, steroids and colchicine-based medications
- NSAIDS decrease local inflammation
Immediately, Advil, Alleve or even indocin can work great. Then, see your podiatrist and have them send you an oral steroid as soon as possible. Rayos or a medrol dose pack are some examples. (Do not use RAYOS if you are allergic to prednisone.) *Do not take NSAIDS and corticosteroids at the same time!
- X-Rays
Most podiatrists have the ability to take an x-ray or radiograpghs at the time of your appointment in the office. It is not necessary to have them taken somewhere else before your visit, and even may delay treatment. This helps to determine what is going on with the joint or bone. We will read this x-ray together with you and determine if what you are having is really an attack of gout.
- Injection of Methylpresnisone decreases pain immediately.
Immediate relief is provided by a cortisone injection directy into the affected joint.
- Sometimes a simple office procedure can alleviate the local pain and deformity.
The podiatrist also can perform aspirations to both treat and verify if a pathological sample is in fact gout crystals.
Excising a deformed small toe joint can also remove an area destroyed by gout crystals. - Krystexxa can help reduce uric acid from the entire body.
Besides a podiatrist and your primary care doctor, a rheumatologist may also help diagnose gout.
The difference is rheumatologists are not as readily available. Their role generally is in more advanced phases of gout, such as chronic gout and long-term medications.
Your podiatrist will work with your primary care doctor and a rheumatologist to create a long-term plan.
For most patients the need and the occasional acute treatment, and do not need long-term treatment.
Other Traditional Gout Treatments
The aim of treatments for gout are to reduce pain and/or inflammation of the attacks or frequency of attacks. Traditional treatments include dietary changes and certain medications.
Gout Diet Modification
Adjusting dietary habits is one of the most important methods to reduce the amount of acute gout attacks. The goal of this is to lower blood levels of uric acid.
The following dietary changes may reduce gout symptoms:
- Reduce or eliminate alcohol
- Drink a lot of water
- Eat low-fat or nonfat dairy products
- Avoid high purine foods
- Limit meat in favor of more plant-based protein sources
- Eat complex carbohydrates such as whole-grains instead of sugary sweets or white bread
Gout Treatment -Medications
The following medications are common gout treatments:
- NSAIDs, corticosteroids, and colchicine may all reduce pain and inflammation associated with acute gout attacks
- Xanthine oxidase inhibitors like allopurinol reduce the amount of uric acid produced in the body
- Probenecid improves the ability of the kidneys to remove uric acid from the bloodstream
If you have gout, there may be signs that a flare-up may be on the way. You cannot stop a gout attack once it starts, but the symptoms may be eased at home.
Types of Gout
Asymptomatic hyperuricemia
It does occur that individuals have elevated uric acid levels without any noticeable symptoms. Treatment is rare at this stage, but urate crystals may deposit into tissue and cause slight damage. We advise those with this asymptomatic condition to take steps to address this uric acid build-up.
Acute Gout
Acute gout is when the urate crystals deposit suddenly and cause inflammation and intense pain. This sudden flare up will typically subside in 3-10 days. Stressful events, alcohol, drugs, and cold weather may trigger these flare ups.

Interval/Intercritical Gout
This stage is the period between flare ups of acute gout. These attacks may not occur again for months or years. Untreated gout may lead to longer and more frequent attacks. More urate crystals deposit into tissue during this stage.
Chronic Tophaceous Gout

This is the most debilitating type of gout to experience. This may be due to permanent damage to the joints and kidneys. Patients may suffer from chronic arthritis and develop tophi and big lumps of urate crystals in cooler areas of the body such as the joints of the fingers. Longterm untreated gout leads to the stage of chronic tophaceous gout and is typically around 10 years. Treated properly, however, a patient would not progress to this stage of gout.
Pseudogout
A condition known as pseudogout is commonly confused with gout. The symptoms are very similar to gout, but the flare-ups of pseudogout are typically less severe. The main difference is that the joints are affected by pyrophosphate crystals rather than urate crystals. The treatment for pseudogout is different from gout treatment.
Causes of Gout
Excess build-up of uric acid in the blood is usually the initial cause of gout, known as hyperuricemia. Uric acid is produced in the body when chemical compounds known as purines are broken down. These are found in high amounts in certain meats, poultry, and seafood. Uric acid is usually dissolved in the blood to be excreted from the body in the urine via the kidneys. When too much uric acid is produced or not enough is excreted, it can form needle-like crystals. This triggers a pain and inflammation response around the joint and surrounding tissues.
Risk Factors of Gout
Various risk factors can increase the likelihood of hyperuricemia which may lead to gout include the following:

- Age and Gender: Men will produce more uric acid than women, but women’s levels of uric acid increase near those of men after menopause.
- Genetics: Family history of gout increases likelihood of condition developing.
- Lifestyle: Alcohol interferes with the body’s ability to remove uric acid. Also, eating a diet that’s high in purines will increase uric acid levels.
- Lead exposure: Gout cases link to Chronic lead exposure
- Medications: Certain medications can increase uric acid levels, such as diuretics and drugs containing salicylate.
- Weight: Individuals who are overweight are at an increased risk of developing gout because of the increased body tissue. First your body gives off more uric acid as a waste product, then higher body fat levels will increase systemic inflammation. Fat cells produce pro-inflammatory cytokines.
- Recent trauma or surgery: Increased risk of developing gout.
Other health problems that can increase uric acid levels in the body are renal insufficiency. This decreases the kidneys’ ability to efficiently remove waste products such as uric acid. High blood pressure and diabetes also increase the likelihood of developing gout.
Symptoms of Gout

Gout typically carries symptoms suddenly without any warning, often during the night. The main symptoms include intense joint pain, discomfort, inflammation, and redness around the area. Gout affects the large joint of the big toe; however, Gout may also affect the forefoot, ankles, knees, elbows, wrists, and fingers.
Warning Signs of a Gout Attack
Individuals with gout may experience burning, tingling, or itching in a joint about an hour prior to a flare-up. The joint may also feel stiff or a bit sore before the gout attack begins. In other cases, people with gout may have no early sign or symptoms that a flare-up is about to start. Waking up in the middle of the night with a very painful joint is common amongst patients with gout.
Once the attack starts, most individuals experience redness, swelling, and severe pain that is focused into one joint. The most common location for gout is in the base of the big toe, but may also occur in other joints such as the elbow, knee, wrist, ankle, and instep.
Home Care for a Gout Flare-Up
If your doctor has diagnosed you with gout and given you medication for a flare-up, take the medication as directed when you know you are having an attack. Your doctor may prescribe NSAIDs such as celecoxib, indomethacin, meloxicam, or sulindac. Over-the-counter NSAIDs such as naproxen or ibuprofen may also be recommended.
Depending on your medical history, your doctor may prescribe steroids or other medicines to reduce inflammation, such as colchicine (Colcrys).
In some cases, your doctor may suggest the following medications to prevent gout flare-ups:
- Allopurinol (Aloprim, Lopurin, Zyloprim)
- Canakinumab (Ilaris Ilaris Ilaris)
- Lesinurad (Zurampic)
- Pegloticase (Krystexxa)
- Probenecid (Probalan)
- Rasburicase (Elitek)
If you cannot take allopurinol or it does not work for your treatment plan, your doctor may prescribe febuxostat (Uloric). This should be used with caution because it has been linked to increased risk of heart disease and death from other complications.
If you experience a flare-up, it doesn’t always mean that the medicine isn’t working. Your body will need time to adjust to the medication, which is why you may experience an attack in the first few months of taking them. Your doctor may give you something to take if this situation occurs.
If you have been using the medication as directed for gout treatment and you experience a new attack for the first time in a while, call your doctor.
Complications of Gout
Gout may develop into more serious conditions such as:
- Kidney stones: Urate crystals may collect in the urinary tract leading to kidney stones
- Recurrent gout: Individuals may have regular recurrences. This causes gradual damage to the joints and surrounding tissues.
Prevention of Acute Gout Attacks

Try these lifestyle and dietary guidelines to protect against flare-ups or prevent gout from starting include the following:
- High fluid intake between 2 and 4 liters of water per day
- Avoid alcohol
- Maintain a healthy body weight
Home Remedies for Gout Treatment
Best Gout Treatment Supplements:
Gout is one of the most misdiagnosed conditions by patients. A Podiatrist should properly diagnosed ypur gout before you administer any treatment at all! Be aware that these supplements may be well rated, but they do lack overall deep scientific evidence.
- cherry concentrate supplement.
- Tumeric
- Biofreeze
- NSAIDS
Patients with gout may manage flare-ups by managing their food and beverage intake. This can help reduce symptoms. Decreasing the foods described.
How does gout affect the joints, and which joints are commonly affected?
Gout primarily affects joints, causing sudden and intense pain, swelling, and redness during flare-ups. The joints most commonly affected are the big toe, ankle, and knee. Gout occurs when urate crystals (formed from high levels of uric acid in the blood) accumulate in joints, triggering an inflammatory response. Over time, repeated flare-ups can lead to joint damage and deformities.
How does alcohol consumption influence gout flare-ups?
Alcohol consumption can significantly influence gout flare-ups due to several reasons:
- Increased Uric Acid Production: Alcohol, especially beer and spirits, can lead to an increase in uric acid production. Elevated uric acid levels are a key factor in the development of gout.
2. Impaired Uric Acid Excretion: Alcohol can interfere with the kidneys’ ability to excrete uric acid effectively. This impairment contributes to the accumulation of urate crystals in the joints, triggering gout attacks.
3. Dehydration: Alcohol is a diuretic, causing increased urine production and potential dehydration. Dehydration concentrates uric acid in the bloodstream, increasing the likelihood of crystal formation in the joints.
4. Purine Content: Certain alcoholic beverages, such as beer and certain wines, contain purines. When metabolized, purines break down into uric acid, contributing to increased uric acid levels in the body.
5. Inflammation and Immune Response: Alcohol can stimulate inflammation and immune responses, potentially exacerbating the inflammatory processes involved in gout flare-ups.
What steps can be taken to alleviate gout pain during a flare-up?
During a gout flare-up, it’s essential to rest the affected joint, elevate it, and apply ice to reduce swelling. Nonsteroidal anti-inflammatory drugs (NSAIDs) or colchicine can help manage pain and inflammation. Staying hydrated and avoiding trigger foods like high-purine items can also aid in symptom relief. Consultation with a healthcare professional is crucial for personalized treatment.
